As a senior editor specializing in neonatal care, I’ve observed the evolution of jaundice screening. Transcutaneous bilirubin (TcB) measurement offers a non-invasive alternative to painful heel pricks. This review explores case studies, analyzes the effectiveness of TcB, highlights inconsistencies in decision rules, and suggests future research directions to refine jaundice screening protocols, particularly for high-risk newborns and those whose mothers experienced pre-eclampsia.
TcB in Neonatal Jaundice Screening: A Critical Analysis of Case Studies
Transcutaneous bilirubinometry (TcB) provides a non-invasive method to estimate bilirubin levels, reducing the need for invasive blood tests. It’s faster, gentler, and less stressful for parents and infants. However, case studies reveal a complex picture of TcB’s accuracy and effectiveness. We explore its benefits, potential drawbacks, and areas needing further investigation. Considering the ease and speed, does TcB represent a significant improvement or a modest advancement in neonatal care?
Accuracy of TcB: Strengths, Weaknesses, and How to Improve Jaundice Screening
Numerous studies demonstrate a strong correlation between TcB and total serum bilirubin (TSB) levels, especially in healthy, full-term infants with lower bilirubin levels. This suggests TcB could significantly reduce the need for invasive blood tests. However, a universally agreed-upon TcB threshold for triggering follow-up blood tests remains elusive. Inconsistent thresholds across different settings and varying false negative rates pose challenges. This is potentially dangerous because undetected high bilirubin levels can lead to severe neurological damage, including kernicterus.
Identifying Cases Where TcB Requires Careful Consideration: Focus on High-Risk Newborns
TcB’s accuracy decreases as bilirubin levels increase, and it can be affected by factors like gestational age, skin pigmentation, and the presence of edema. In cases of severely elevated bilirubin, TcB alone is insufficient, necessitating confirmation with TSB tests. Emerging research indicates that maternal conditions, such as pre-eclampsia, may influence TcB readings in newborns, potentially leading to inaccurate estimations. Further investigation is needed to clarify these relationships and refine screening protocols. Are we overlooking crucial factors affecting TcB accuracy in vulnerable populations?
One study from Slovakia involving 102 jaundiced term Caucasian neonates found that transcutaneous measurements consistently underestimated serum bilirubin levels, especially when TSB values exceeded 15 mg/dL. This underestimation highlights the importance of verifying high TcB readings with TSB measurements.
Pursuing Standardization and Research for Reliable TcB Results: Improving Neonatal Care
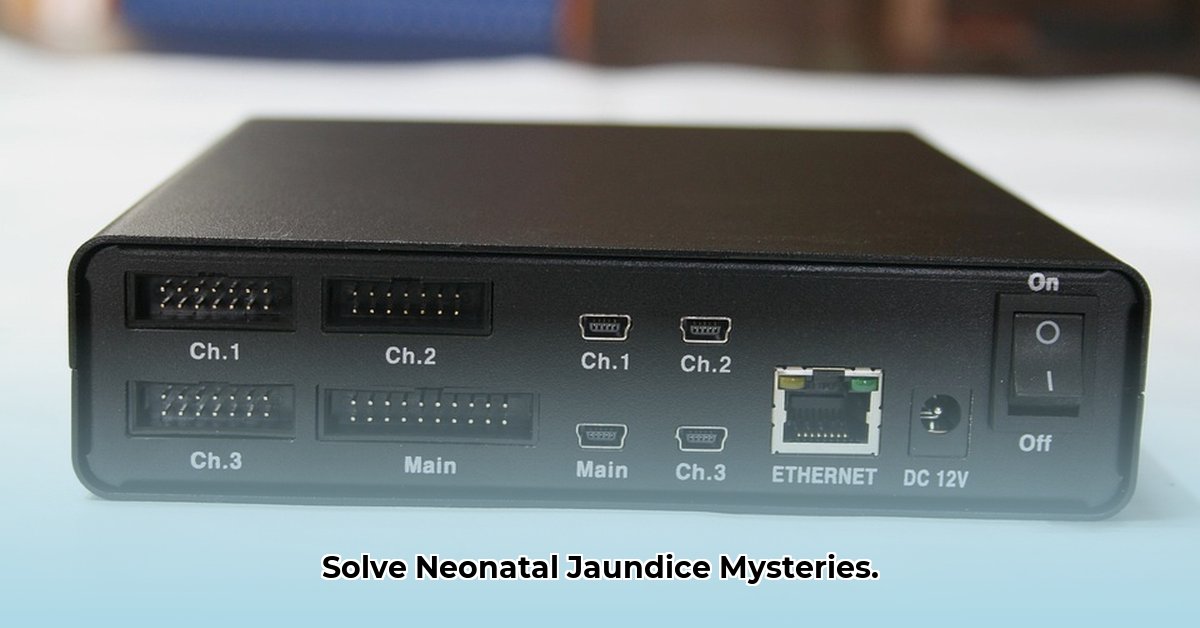
A significant challenge facing TcB is the lack of standardized procedures and equipment, leading to variability in results. Factors such as the type of device used, the measurement site (forehead, sternum), and the technique of the operator can all influence TcB readings. Scientists and clinicians are actively working to address this issue by developing improved devices and consistent testing techniques. Future research focuses on personalizing decision rules based on factors like gestational age, birth weight, ethnicity, and maternal health conditions, optimizing screening for each infant.
Practical Guidelines for Healthcare Professionals: Optimizing the Use of TcB Scans
Healthcare professionals can take the following steps to optimize their use of TcB in jaundice screening:
- Stay Informed: Remain current with the latest research findings and clinical guidelines regarding TcB performance, particularly in high-risk populations.
- Utilize Standardized Protocols: Adhere to standardized TcB measurement protocols, including proper device calibration, consistent measurement sites (forehead or sternum), and appropriate skin preparation.
- Interpret with Caution: Interpret TcB results cautiously, considering factors that may affect accuracy, such as gestational age, ethnicity, and maternal conditions.
- Verify High Readings: Always verify high TcB readings with TSB measurements, especially when TcB values approach or exceed established thresholds.
- Maintain Detailed Records: Meticulously document TcB results alongside TSB values (when available) to evaluate the effectiveness of different decision rules for specific patient populations.
- Apply Cautiously: Integrate TcB into clinical practice carefully, acknowledging its limitations, especially in high-risk situations.
- Foster Collaboration: Share findings and insights with colleagues to enhance understanding and improve treatment strategies collectively.
Data-Driven Solutions: TcB Pros & Cons
| Advantage | Disadvantage |
|---|---|
| Non-invasive and kinder to the baby | Less accurate with very high bilirubin levels |
| Faster results | Inconsistent guidelines for follow-up blood tests |
| Potentially reduces the need for blood tests | May be affected by gestational age, ethnicity, and maternal health conditions |
| Cost-effective | Needs better standardization |
In conclusion, TcB offers a promising non-invasive approach to neonatal jaundice screening. Realizing its full potential requires ongoing research, standardization of methods, and clearly defined guidelines, especially for high-risk newborns. As the field evolves, continuous investigation and refinement are essential to maximize the benefits of TcB while minimizing potential risks.
Adjusting Transcutaneous Bilirubin Screening for High-Risk Newborns: A Tailored Approach
Early jaundice detection prevents severe complications. Transcutaneous bilirubin (TcB) measurements provide a valuable non-invasive screening method, but how to adjust transcutaneous bilirubin screening for high-risk newborns requires careful consideration given the factors affecting accuracy. Establishing optimal decision rules for TcB interpretation remains a challenge, and standardization of protocols across healthcare is essential.
Navigating TcB Screening Challenges in High-Risk Infants: Assessing Unique Needs
Neonatal jaundice, characterized by yellowing of the skin and eyes, signals hyperbilirubinemia. While often benign, severe hyperbilirubinemia can lead to kernicterus and permanent neurological damage. Early detection is paramount. TcB offers a non-invasive screening method, but its accuracy can be affected, especially in high-risk infants. Does this variability compromise TcB’s reliability, and how can we mitigate these risks?
High-risk newborns (prematurity, low birth weight, birth trauma, underlying conditions such as hemolytic disease) present unique challenges. Variations in skin pigmentation, hydration, and perfusion affect TcB accuracy. Therefore, how to adjust transcutaneous bilirubin screening for high-risk newborns requires a nuanced and individualized approach. Is this variability worth the risk of diagnostic error, and what strategies can improve accuracy in these cases?
Precision Screening: A Strategic Plan for High-Risk Infants
Effective management requires a multi-faceted and strategic plan:
- Risk Stratification: Identify high-risk newborns early through careful evaluation of gestational age, birth weight, underlying conditions, and maternal history.
- TcB Technique: Standardize TcB measurement procedures to minimize variability. Use calibrated devices, select consistent measurement sites (forehead or sternum), and ensure proper skin preparation. Avoid areas with bruising or excessive hair.
- Interpretive Decision Rules: Clinicians may need to adjust interpretation criteria based on risk profiles. Lower thresholds for TSB confirmation may be warranted in preterm infants or those with hemolytic disease.
- Integration with Other Measures: TcB serves as a screening tool, and abnormal results require prompt total serum bilirubin (TSB) measurement to confirm diagnosis and guide treatment. Consider using a TSB nomogram to assess the risk of hyperbilirubinemia based on the infant’s age in hours.
- Clinical Correlation: Always consider the clinical picture. Evaluate the infant for signs of jaundice, feeding difficulties, and lethargy.
Addressing Gaps in Current TcB Screening Practices: Reducing Discrepancies
Discrepancies exist in guidelines and protocols for managing neonatal hyperbilirubinemia, particularly for high-risk infants. Optimal TcB decision rules requiring confirmatory TSB remain debated. Research is needed to establish universally accepted thresholds specific to high-risk groups, potentially improving screening efficacy.
The Future of TcB Screening in Neonatal Jaundice Management: Research and Development
TcB remains valuable in neonatal hyperbilirubinemia management. Research aims to improve accuracy and reliability, refining decision rules, improving device calibration, and developing algorithms incorporating additional clinical parameters. This is crucial because the Impact of Maternal Pre-eclampsia on Neonatal TcB Accuracy and Screening directly influences treatment decisions.
TcB Screening Protocols for Preterm Infants with Pre-eclampsia: A Specialized Approach
Effective and specialized protocols are essential to improve the screening of preterm infants, especially those born to mothers with pre-eclampsia, to combat jaundice. Transcutaneous bilirubinometry (TcB) offers a non-invasive alternative to traditional blood tests for assessing jaundice in newborns, particularly preterm infants, reducing discomfort and infection risk. TcB Screening Protocols for Preterm Infants with Pre-eclampsia require careful consideration, recognizing the potential impact of pre-eclampsia on bilirubin levels and the unique challenges of assessing jaundice in this vulnerable population.
Tcb Scans: An Imperfect Technology Requiring Careful Application?
TcB uses a sensor to estimate bilirubin levels through the skin quickly. But its accuracy isn’t perfect, especially in preterm infants. Why? Their skin is thinner and less mature, which can affect the readings. Preterm infants with pre-eclampsia present added complexities because pre-eclampsia can affect liver function, potentially skewing TcB results. This necessitates careful interpretation and potentially confirmatory blood tests.
Key Considerations for Preterm Infants with Pre-eclampsia: Gestational Age, Maternal Condition, and Ethnicity
Gestational age significantly influences TcB accuracy. The younger the infant, the less reliable the TcB reading often is. This is because skin development and bilirubin metabolism vary with gestational age.
Recognizing pre-eclampsia is crucial. This pregnancy
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026