Ever heard of TCB scans? They’re a non-invasive way to gain insights into the body, offering a new perspective on how we diagnose and treat illnesses. For more detailed information, see this helpful guide on [TCB scans](https://txgenco.com/what-are-tcb-scans). This guide breaks down everything you need to know about understanding TCB scan reports, from how they work to what the results mean. Whether you’re a healthcare provider, a technician, or simply curious, we’ll make this easy to understand. We’ll cover interpreting results, comparing them to other tests, and how to use this technology to improve patient care. Let’s explore the world of TCB scans.
Decoding TCB Scan Reports
Understanding TCB scan reports can seem complicated, but this guide will break down this technology, its uses, and what’s needed to interpret its results. Consider this your go-to explainer for TCB scans, giving you insights into medical imaging and diagnostic tools.
What are TCB Scans? A Non-Invasive Examination
TCB, or transcutaneous biophotonic, scans offer a non-invasive method for doctors to examine the body. This technique uses light to create images of tissues. This enables earlier disease detection, better diagnoses, and improved treatment plans. As a relatively new technology, it has challenges necessitating ongoing development and refinement.
How Do TCB Scans Work? The Power of Light
TCB scans use light’s interaction with the body’s tissues. Tissues absorb and reflect light differently, and the TCB scanner measures these differences to build an image. Different types of TCB scanners highlight specific factors during an examination, such as blood flow, oxygen levels, or certain tissue characteristics. Specialized equipment allows for precision measurements.
Applications of TCB Scans in Healthcare
This technology has a wide range of potential uses. Doctors can use it to check bone health, look for tumors, or monitor newborns for jaundice. Successful trials include pain management, diagnosing headaches, and pinpointing tumors more accurately, which leads to better treatment decisions. While some applications are more established than others, further research is needed in some areas before they are used routinely, thus warranting careful consideration for various medical scenarios. Specific applications include:
- Oncology: Detecting bone metastases and monitoring treatment response in cancer patients.
- Infectious Diseases: Diagnosing osteomyelitis and monitoring treatment response.
- Orthopedics: Diagnosing bone fractures, avascular necrosis, and Paget’s disease.
- Neonatal Care: Measurement of bilirubin levels in newborns.
- Cardiology: Assessing cardiac and vascular health.
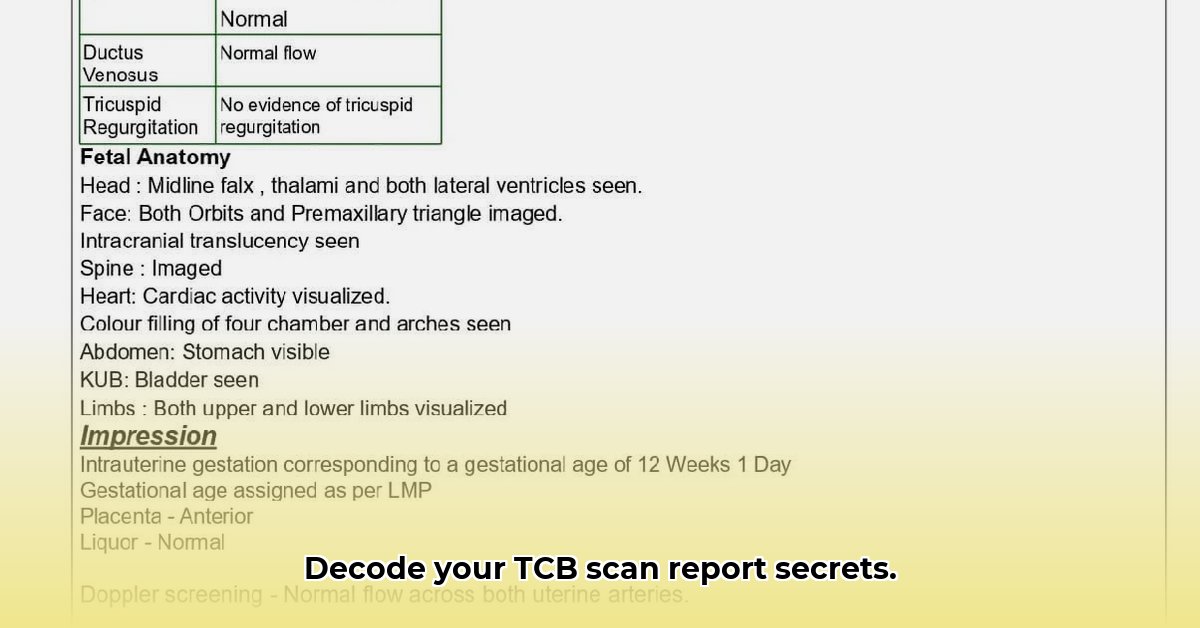
Reading the Report: More Than Just an Image
Interpreting a TCB scan report requires trained professionals because the reports contain significant amounts of information, including numbers and visual representations that require expert analysis. Standardized procedures and ongoing training are critical because misinterpretation can mean misdiagnosis or delayed treatment.
Challenges and Limitations of TCB Scans
TCB scans have several challenges. Accuracy is a major concern, and some studies have shown that the reliability of the results may vary depending on a patient’s skin tone. Cost is another obstacle because TCB scans aren’t widely available, and smaller healthcare facilities might not have access to them. Also, regulations vary depending on location and the intended use of the technology, which affects how quickly it can become a standard tool in healthcare.
Innovations and the Future of TCB Scans
The future of TCB scans is promising. Scientists are working on improving accuracy while reducing costs. Integrating artificial intelligence (AI) could change how images are analyzed, potentially leading to faster and more accurate diagnoses. Also, miniaturizing the scanners would make them more portable, improving access for patients in remote areas or those unable to easily get to a hospital. To make this technology commonplace will require further clinical trials and clearer professional guidelines, including enhanced data analysis and greater access. Specific innovations include:
- AI-enhanced analysis: Improved image analysis accuracy and diagnostic speed.
- Molecular imaging: Increased sensitivity and specificity of TCB scans.
- Telemedicine integration: Patients consult specialists using real-time data from TCB scans.
Actionable Steps for Progress
Here’s how different groups can help advance the use of TCB scans:
| Stakeholder Group | Short-Term Actions | Long-Term Actions |
|---|---|---|
| Healthcare Providers | Invest in training to interpret reports. | Standardize procedures for TCB scans across specialties. |
| Medical Technology Companies | Improve accuracy, lower costs, and develop smaller scanners. | Develop AI-powered systems for automatic analysis and diagnosis. |
| Regulatory Bodies | Streamline approval processes for applications. | Develop clear standards and guidelines for use and interpretation of the scan reports. |
| Patients | Learn about TCB scans and their benefits. | Advocate for better access and lower prices. |
| Researchers | Conduct trials to test accuracy. | Explore new applications, such as molecular imaging and personalized medicine. |
Understanding Potential Risks
It’s important to understand potential risks and how to mitigate them:
| Aspect | Potential Risk Level | Mitigation Strategies |
|---|---|---|
| Accuracy | Moderate | Ongoing technological advancements and rigorous testing and validation. |
| Cost | High | Subsidies, economies of scale, and development of more affordable devices. |
| Accessibility | Moderate | Targeted distribution and focused training programs. |
| Regulatory Hurdles | Moderate | Proactive engagement with regulatory agencies. |
| Patient Discomfort | Low | Non-invasive procedure to minimize any potential discomfort. |
| Contrast Agent Reactions | Low | Pre-screening and careful monitoring using established best practices. |
| Radiation Exposure | Negligible | Use of minimal radiation doses (when applicable) and appropriate shielding when radiation is used. |
This guide demystifies TCB scan reports, presenting both opportunities and challenges. It’s relevant for professionals, researchers, and patients interested in this field. The information here reflects current understanding, and ongoing research may further refine understanding of TCB scans and technological innovations.
Improving Accuracy for Diverse Skin Tones
Key Takeaways:
- Transcutaneous bilirubin (TcB) measurements are affected by skin pigmentation, and darker skin tones can lead to underestimation.
- Algorithms and device calibrations are crucial for accurate measurements across all skin tones.
- Factors beyond skin tone, such as skin thickness, hydration, and bone structure, also influence accuracy, especially in premature infants.
- Collaboration between device manufacturers, clinicians, and researchers is essential for advancing TcB technology through rigorous analysis and improvement.
Challenges in TcB Measurements
TCB scans offer a way to check bilirubin levels in newborns without needles, which is helpful in screening for jaundice. However, achieving accuracy across different skin tones is a challenge. Melanin, the pigment responsible for skin color, impacts light absorption and penetration, leading to variability in TcB readings and underestimation of true bilirubin levels, particularly in infants with darker skin.
Factors Influencing Accuracy
Several factors affect TcB accuracy beyond skin pigmentation, including skin thickness, hydration levels, and even bone structure, and premature babies are particularly vulnerable to inaccurate readings. This complexity highlights the importance of developing more sophisticated measurement methods to provide accurate diagnostics for all newborns.
Strategies for Improving Accuracy
Improving TCB scan accuracy for diverse skin tones requires a collaborative effort. Device manufacturers must create algorithms that account for variations in skin pigmentation and other anatomical nuances. This might involve incorporating multiple wavelengths of light for more accurate analysis. Clinicians can improve outcomes by considering skin tone when interpreting TcB results and supplementing with blood tests when necessary. Further research is needed to develop accurate and robust models for predicting bilirubin levels across a diverse population.
Steps Towards Better Accuracy
Here’s a breakdown of actionable steps:
- Refined Algorithms: Device manufacturers should develop algorithms that compensate for the effects of melanin, skin thickness, and other variables.
- Calibration Improvements: Standardized calibration procedures should be appropriate for a range of skin tones.
- Multi-Ethnic Trials: Clinical trials incorporating diverse populations are essential to validate new technologies and ensure equitable diagnostic accuracy.
Additional Resources
- American Academy of Pediatrics guidelines on hyperbilirubinemia.
- National Institute of Child Health and Human Development (NICHD) research on neonatal jaundice.
- World Health Organization (WHO) resources on newborn health.
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026