Newborn jaundice is a common condition that requires prompt and accurate diagnosis to prevent potential complications. This review article compares transcutaneous bilirubin (TcB), a non-invasive skin measurement, with total serum bilirubin (TSB), a blood test, for assessing neonatal jaundice. We will explore the advantages and limitations of each method, addressing the influence of factors like skin tone and gestational age on TcB readings, and provide guidance on interpreting test results, ultimately aiding healthcare providers and parents in making informed decisions regarding jaundice diagnosis and management. The overarching goal is to minimize the need for invasive blood tests while ensuring accurate and timely intervention and reducing parental anxiety. For more information on bilirubin level scans, see this helpful resource.
Understanding Neonatal Jaundice: Comparing TcB and Serum Bilirubin Testing Methods
The accurate assessment of bilirubin levels is paramount in managing newborn jaundice. Two primary methods are employed: transcutaneous bilirubinometry (TcB) and serum bilirubin (TSB) measurement. This section will dissect each method, elucidating the rationale behind selecting the appropriate approach for individual cases. Considerations include the baby’s age, gestational maturity, and any existing risk factors for hyperbilirubinemia. What are the key differences between these jaundice detection methods, and how do they impact clinical decisions?
Transcutaneous Bilirubin (TcB): A Non-Invasive Screening Tool for Jaundice
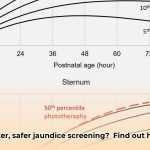
TcB involves shining a light on the baby’s skin (typically the forehead or sternum) using a specialized device that estimates bilirubin levels non-invasively. The device analyzes the light reflected from the skin, and calculates a bilirubin level. This method is prized for its rapid results (typically available in seconds) and ease of use, eliminating the need for needles and blood draws. Are there limitations to the widespread adoption of TcB in accurately diagnosing neonatal jaundice?
Serum Bilirubin (TSB): The Gold Standard for Jaundice Measurement
Serum bilirubin measurement requires a small blood sample, usually obtained via heel prick, to precisely quantify bilirubin levels. The blood sample is sent to a laboratory for analysis. This invasive procedure is considered the gold standard due to its accuracy but takes longer (results may take several hours) and involves a needle prick, which can be distressing for the infant. How can we improve the patient experience surrounding serum bilirubin testing, making it less distressing for newborns and their families?
Advantages of Transcutaneous Bilirubin (TcB): Speed, Convenience, and Reduced Blood Draws
TcB offers rapid results, providing near-instantaneous bilirubin estimates. Its non-invasive nature minimizes discomfort for newborns and streamlines the testing process for healthcare professionals. Newborns often cry less during TcB measurement compared to blood draws. In addition, TcB can help reduce the need for blood tests, minimizing the risk of infection and anemia, particularly in preterm infants who may require frequent bilirubin monitoring. Can TcB replace invasive blood draws as the primary method for neonatal jaundice detection, and what technological advancements are needed to achieve this?
Limitations of Transcutaneous Bilirubin (TcB): Accuracy and Skin Tone Variability
TcB may produce false positives or false negatives. Accuracy can also be influenced by skin tone, gestational age, postnatal age, device calibration, and technique leading to inconsistent readings. Studies have shown that TcB tends to overestimate TSB in preterm infants and underestimate TSB in newborns with darker skin tones. This is due to melanin interfering with the light reflection and absorption used by the TcB device. TcB readings may also be unreliable after phototherapy. As an example, one study showed that TcB overestimated TSB levels in preterm infants with darker skin by an average of 1.2 mg/dL. How can we address the biases inherent in TcB technology to ensure equitable healthcare outcomes for newborns of all racial and ethnic backgrounds?
Comparative Analysis: TcB vs. Serum Bilirubin for Jaundice Detection
| Feature | TcB | Serum Bilirubin |
|---|---|---|
| Method | Non-invasive, skin measurement | Invasive, blood test |
| Speed | Very fast (seconds) | Slower, needs lab processing (hours) |
| Pain | Painless | Painful (heel prick) |
| Sensitivity | Excellent at finding potentially high levels | Excellent at measuring bilirubin accurately |
| Specificity | Lower; more false positives, more false negatives | Higher; fewer false positives |
| Accuracy | Can vary; influenced by skin tone, gestational age, technique etc. | More accurate; considered the gold standard |
| Cost | Generally lower | Generally higher (blood draw, lab work) |
| Risk | Negligible | Risk of infection, anemia (with repeated draws) |
Optimizing Jaundice Management: A Sequential Approach
A common approach involves using TcB as a first-line screening tool. Elevated TcB readings, or readings that are inconsistent with the clinical picture, are then confirmed with a serum bilirubin test. This sequential strategy leverages the speed and non-invasive nature of TcB and the accuracy of serum bilirubin for comprehensive jaundice management. The American Academy of Pediatrics recommends that all newborns be screened for jaundice before discharge from the hospital, using either TcB or TSB. Given the evolution of diagnostic technologies, what innovative strategies can we employ to optimize the accuracy and efficiency of neonatal jaundice screening programs?
Advancing TcB Technology: The Future of Jaundice Detection
Ongoing research aims to enhance TcB accuracy, particularly for babies with diverse skin tones and varying gestational ages. Improved calibration techniques, multiple wavelength analysis, and sophisticated algorithms hold promise for creating a universally reliable and equitable test. Specifically, researchers are exploring methods to correct TcB readings based on skin melanin content. What emerging technologies, such as artificial intelligence and machine learning, can be leveraged to further refine TcB precision and reliability?
Addressing Racial Disparities: Skin Tone and Bilirubin Measurement
Studies have revealed that TcB accuracy varies across different racial groups, potentially leading to disparities in treatment. Addressing this issue requires the development of more precise tools that accurately measure bilirubin levels in all babies, irrespective of skin color. This includes developing and implementing algorithms that account for skin pigmentation. Furthermore, healthcare providers should be aware of these limitations and use clinical judgment when interpreting TcB results in newborns with darker skin tones. How can we foster greater collaboration between researchers, clinicians, and policymakers to mitigate racial biases in jaundice diagnosis and treatment?
Strategies for Enhanced TcB Accuracy in Newborns with Darker Skin Tones
Transcutaneous bilirubin (TcB) offers a non-invasive, cost-effective approach to screening for neonatal jaundice, serving as an alternative to traditional serum bilirubin (TSB) testing. While TcB accuracy is generally reliable for term infants, it can vary in preterm neonates, particularly those with darker skin tones, where TcB often overestimates TSB levels. Several factors contribute to this variability, including the influence of melanin, gestational age, and device limitations. What innovative methods are emerging to address these variations and enhance the reliability of TcB across diverse populations?
Key Insights:
- TcB presents a non-invasive, cost-effective alternative to traditional serum bilirubin (TSB) testing.
- TcB is generally accurate for term infants, when used and interpreted correctly.
- TcB is less accurate for preterm infants and newborns with darker skin, often overestimating TSB, and sometimes underestimating TSB.
Understanding the Influence of Melanin: TcB Challenges
Melanin, the pigment responsible for skin color, interferes with light absorption, influencing TcB readings. This interference is particularly pronounced at the wavelengths traditionally used by TcB devices. This effect is particularly relevant in preterm infants, who are vulnerable to severe jaundice. Is there a non-invasive technique that can accurately measure melanin concentrations in newborn skin, allowing for the fine-tuning of TcB algorithms to enhance precision?
Strategies for Accurate Jaundice Screening
Several strategies are being investigated and implemented to improve the effectiveness of TcB in newborn jaundice assessment:
- Advanced TcB Technology: Newer TcB devices are equipped with improved optical sensors and algorithms designed to minimize the interference of skin pigmentation, offering more reliable measurements across diverse skin tones. For example, some incorporate dual-wavelength spectrophotometry or multi-wavelength spectral analysis to differentiate between bilirubin and melanin absorption. Some devices also incorporate ambient light sensors to further refine accuracy. The key is to use devices validated for use in diverse populations.
- Calibration and Standardization: Consistent results depend on rigorous and frequent calibration of TcB devices using manufacturer-provided calibration modules. Standardizing measurement techniques and protocols across healthcare settings reduces variability and improves measurement accuracy. Proper technique includes gentle pressure and avoiding areas with bruising or birthmarks. Studies show that standardized protocols can improve accuracy.
- Gestational Age and Postnatal Age Adjustment: Accounting for gestational age and postnatal age is vital, as these factors significantly impact bilirubin production and clearance. Algorithms are being developed to adjust TcB readings based on gestational age and postnatal age, improving the correlation with TSB levels, especially in preterm infants. Such adjustments have shown a reduction in false positive results and can improve positive predictive value.
- Population-Specific Reference Intervals: Establishing separate reference intervals for TcB based on gestational age, postnatal age, and skin tone enhances result interpretation, leading to better clinical risk prediction. Adjusted ranges can reduce the need for unnecessary blood draws. This requires ongoing research and data collection to establish appropriate norms.
- Combined Measurements and Clinical Assessment: Integrating TcB with other clinical indicators, such as visual assessment for jaundice, gestational age, birth weight, feeding history, and family history of jaundice
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026