Decoding Your Thumb’s MVP: The MP Joint
Your thumb’s remarkable dexterity hinges on a small but mighty joint at its base: the metacarpophalangeal (MP) joint. This guide explores the MP joint’s anatomy, function, common problems, and how these problems are diagnosed and treated. Whether you’re experiencing thumb pain or simply curious, this guide provides valuable insights into maintaining thumb health.
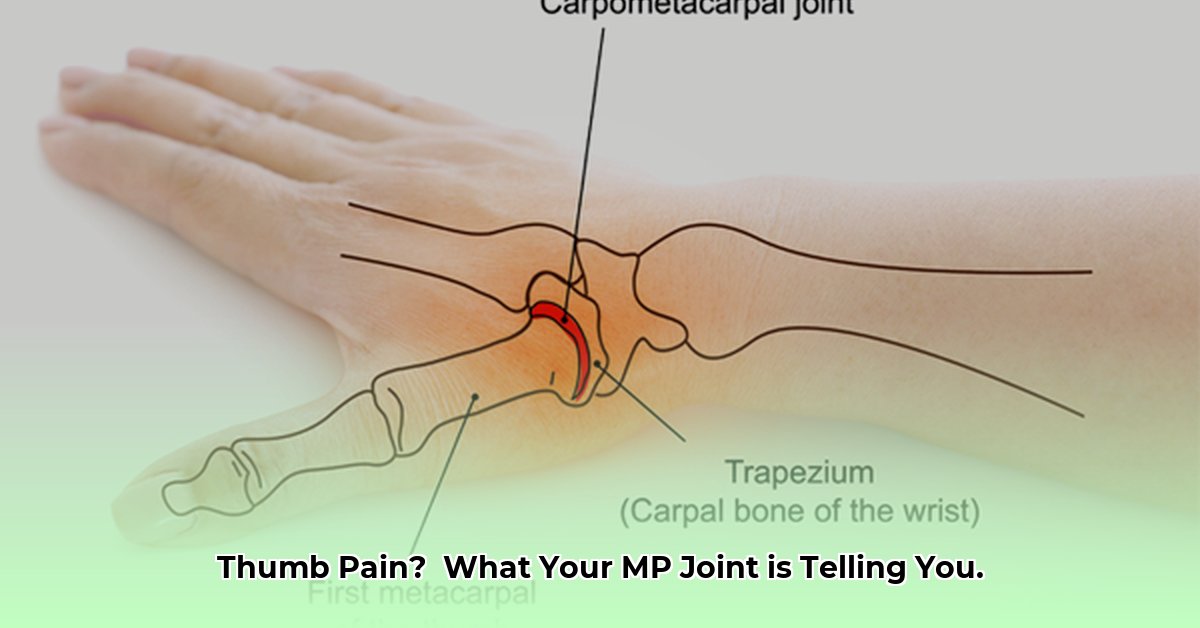
Anatomy and Biomechanics: The Inner Workings of Your Thumb
The thumb MP joint connects the metacarpal bone (in your palm) to the proximal phalanx (the first bone in your thumb). Unlike a simple hinge, this condyloid joint allows movement in multiple directions, enabling bending, straightening, rotation, and movements toward and away from your palm. This versatility is essential for gripping, pinching, and fine motor skills.
Ligaments: The Joint’s Stabilizers
Strong ligaments, acting like ropes, support the MP joint:
- Ulnar Collateral Ligament (UCL): Stabilizes the inner side, preventing excessive outward bending. Injury to this ligament is common, sometimes called “Skier’s Thumb.”
- Radial Collateral Ligament: Stabilizes the outer side, preventing excessive inward bending
- Palmar Ligament: Limits backward bending.
Muscles and Movement: Powering the Thumb
Muscles surrounding the MP joint provide the power for movement:
- Flexor Pollicis Brevis and Longus: Bend the thumb.
- Extensor Pollicis Brevis and Longus: Straighten the thumb.
- Abductor Pollicis Brevis and Longus: Move the thumb away from the palm.
- Adductor Pollicis: Moves the thumb toward the palm.
This coordinated muscle action enables the precise movements we rely on daily.
Common Problems: When Your Thumb Aches
Several conditions can affect the thumb MP joint:
Arthritis: The Joint’s Nemesis
- Osteoarthritis: “Wear-and-tear” arthritis, resulting from cartilage breakdown. Symptoms may include gradual pain, stiffness, limited movement, and a grating sensation.
- Rheumatoid Arthritis: An autoimmune disease causing inflammation of the joint lining. Symptoms can resemble osteoarthritis but often involve more swelling and may affect other joints.
- Psoriatic Arthritis: Another autoimmune arthritis, often accompanied by skin changes.
Injuries: From Sprains to Fractures
- Sprains: Stretched or torn ligaments, often caused by sudden force. Symptoms include pain, instability, weakness, and bruising.
- Strains: Injured muscles or tendons.
- Fractures: Broken bones, usually from direct impact. Symptoms include severe pain, swelling, and possible deformity.
- Dislocations: Bones forced out of their normal position.
Other Conditions:
- De Quervain’s Tenosynovitis: Inflammation of wrist tendons, pain may radiate to the thumb.
- Trigger Thumb: A tendon problem causing the thumb to catch or lock.
- Gout and Pseudogout: Crystal deposits in the joint causing sudden, severe pain and swelling.
Diagnosis: Pinpointing the Problem
If you experience persistent thumb pain, consult a doctor or hand specialist. They will likely:
- Conduct a physical exam: Checking for tenderness, swelling, and range of motion limitations.
- Order imaging tests: X-rays are common, sometimes MRIs or CT scans are needed for a detailed view.
- Consider blood tests: To rule out other conditions or assess inflammation.
Treatment: Restoring Comfort and Function
Treatment depends on the specific condition and its severity.
Non-Surgical Options:
- Rest and Splinting: Immobilizing the joint to promote healing.
- Ice and Heat: To reduce pain and swelling.
- Medication: Over-the-counter pain relievers or prescription medications.
- Injections: Corticosteroids injected into the joint to reduce inflammation.
- Occupational Therapy: Exercises to improve range of motion, strengthen muscles, and develop adaptive techniques.
Surgical Options:
- Joint Fusion (Arthrodesis): Fusing the bones for pain relief, but with some loss of motion.
- Joint Replacement (Arthroplasty): Replacing the damaged joint with an artificial one.
- Ligament Reconstruction and Tendon Interposition (LRTI): Reconstructing the ligaments for stability.
- Trapeziectomy: Removing a wrist bone to relieve pressure and pain.
Recovery and Beyond
Recovery after surgery involves physical therapy to regain strength and function. Assistive devices can help with daily tasks.
Ongoing Research and Uncertainties
Research continues to explore the biomechanics of the thumb MP joint and refine treatment approaches. For example, the role of genetic factors in arthritis development is being investigated, and the optimal balance between conservative and surgical treatments remains a topic of discussion among experts.
When to Seek Medical Attention
Consult a doctor if your thumb pain is:
- Severe
- Persistent (lasting more than a few weeks)
- Accompanied by swelling, redness, warmth, or limited movement
- Interfering with daily activities
Disclaimer: This information is for educational purposes only and does not constitute medical advice. Always consult a healthcare professional for any health concerns.
- NYC BBL Lookup: Master Property Records & Taxes Now - June 30, 2025
- Experience Blue11: Caribbean Fine Dining Review - June 30, 2025
- Berendsen Fluid Power Solutions: Boost Efficiency Now - June 30, 2025