Checking for jaundice in newborns is essential and helps prevent serious complications. This article rigorously examines devices that measure bilirubin levels through the skin (TcB), offering practical advice for accurate readings and comparing different technologies. The aim is to assist healthcare professionals in providing the best possible care for newborns at risk of hyperbilirubinemia. For more on TcB accuracy, see this helpful resource: TcB accuracy study.
Transcutaneous Bilirubin Device Reviews: Getting the Jaundice Read Right
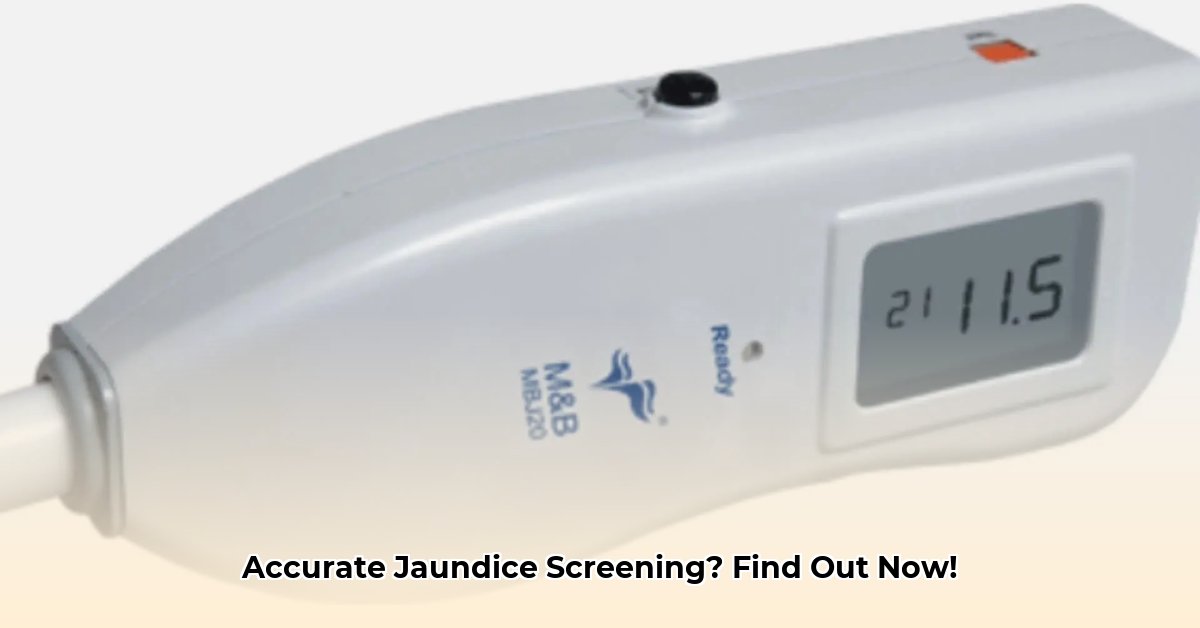
Checking for jaundice in newborns is crucial, and transcutaneous bilirubin (TcB) devices offer a non-invasive way to do this without the need for a blood test. These devices offer a convenient alternative for initial screening. But how accurate are they? Let’s delve into the world of TcB device reviews and explore their effectiveness in neonatal jaundice assessment. Understanding the limitations of bilirubin measurement is crucial for effective neonatal care and preventing kernicterus.
The Accuracy Question: Hitting the Mark with TcB
Reviews of TcB devices reveal a range of accuracy. While undeniably convenient, variations exist across different devices and clinical scenarios. This means that while TcB offers a rapid and painless screening tool, healthcare providers must be aware of the potential for both false positives (leading to unnecessary blood tests) and false negatives (potentially delaying treatment). It’s essential to consider factors affecting jaundice detection to minimize errors and ensure appropriate intervention.
The challenge lies in establishing universally accepted and reliable “trigger points” for intervention. While TcB readings can provide valuable insights, determining the precise cutoff value that warrants confirmatory blood testing remains a subject of ongoing research and refinement. The lack of a definitive “magic number” underscores the importance of integrating TcB measurements with clinical judgment and consideration of individual patient factors.
What Influences the Reading? Beyond the Device Itself
Several factors can affect how accurately a TcB device measures bilirubin levels. Babies born prematurely, for instance, might give slightly different readings than full-term infants. The baby’s skin color plays a role too – darker skin tones can impact the reading. Gestational age, postnatal age, body weight, and even the specific site of TcB measurement can influence the results. Proper device calibration and technique are also paramount to obtaining reliable measurements. Accurate readings depend on precise jaundice screening methods.
Comparing Devices: A Landscape of Options
Several TcB devices are available, each with its own characteristics and performance profile. While reviews offer some comparative insights, more comprehensive research is needed across diverse populations, including those with varying ethnic backgrounds, gestational ages, and clinical conditions. Individual institutions should perform their own evaluations of different devices to determine the best option for their patient population. Below is a preliminary comparison based on available data. Remember, this isn’t exhaustive – further research is always needed to get the complete picture.
| Device | Pros | Cons |
|---|---|---|
| SpectRx BiliCheck | Easy to use, portable, makes testing convenient. | Readings can be quite variable, leading to potential inaccuracies. Requires disposable calibration tips, contributing to ongoing costs. |
| Minolta AirShields JM-102/103/105 | Long-standing technology, widely used and familiar to many clinicians. Non-invasive and provides rapid results. | Readings can be quite variable, leading to potential inaccuracies. May be affected by ambient light. |
Improving the Use of TcB: Best Practices for Success
To maximize the usefulness of TcB devices and minimize errors, a multi-faceted approach is necessary.
- Choose Wisely: Select devices known for their accuracy and reliability. Reviews and independent testing should guide your selection. Consider devices that have demonstrated consistent performance in studies involving diverse populations.
- Establish Clear Guidelines: Create very specific instructions on how to interpret TcB readings and what actions to take based on those readings. Develop algorithms that incorporate gestational age, ethnicity, and other relevant clinical factors.
- Invest in Excellent Training: Staff need comprehensive training on using the device properly. Consistent and accurate results won’t happen without skilled hands. Regular refresher courses are also beneficial. Training should emphasize proper technique, calibration procedures, and awareness of potential sources of error.
- Collaboration is Key: Work with other healthcare professionals to improve the technology and establish universally accepted guidelines. Share best practices and participate in collaborative research efforts to refine TcB protocols.
- Regular Calibration and Maintenance: Adhere to the manufacturer’s recommendations for device calibration and maintenance. Regular calibration ensures accurate measurements of controls and reduces the risk of device malfunction.
The Road Ahead: Future of TcB in Neonatal Care
While TcB devices are a convenient tool, ongoing research needs to tackle their limitations. This includes the development of more accurate sensors and algorithms that can better account for factors like skin tone and gestational age. Better standardization across devices would be a huge step forward, too. Integration of machine learning algorithms may hold promise for improving accuracy and reliability. Can future technologies mitigate current limitations in bilirubin measurement?
Some experts believe that technological advancements are likely to significantly improve accuracy in the future. However, even with these improvements, it’s unlikely that TcB will entirely replace traditional blood tests for bilirubin measurements. Instead, TcB is best viewed as a valuable screening tool that can improve efficiency, reduce the need for blood draws, and facilitate early detection of hyperbilirubinemia. Therefore, understanding its limitations and properly integrating TcB into clinical practice is incredibly important. The future of TcB looks bright but depends on ongoing research and collaborative efforts to establish evidence-based guidelines and better devices.
How to improve transcutaneous bilirubinometry accuracy in premature infants
Key Takeaways:
- Transcutaneous bilirubinometry (TcB) offers a non-invasive alternative to traditional blood tests for jaundice screening in newborns, especially premature infants.
- While TcB correlates well with serum bilirubin levels, accuracy can vary, particularly in very premature infants due to factors such as skin immaturity and variations in bilirubin distribution.
- Cost savings and reduced patient discomfort are significant advantages of TcB, making it an attractive option for routine screening in neonatal intensive care units (NICUs).
Understanding the Challenges of TcB in Premature Infants
Accurately measuring bilirubin levels in premature infants is crucial for preventing severe jaundice and its potential neurological complications. Traditional methods, involving repeated blood draws, are invasive and risky for these vulnerable newborns. TcB offers a less invasive alternative, but its accuracy can be affected by several factors. The biggest challenges? Premature infants often have thin, delicate skin which affects readings. Their immature physiology can also introduce variability. Furthermore, preemies are at higher risk for hypotension and other conditions that can influence TcB measurements. Optimizing jaundice management in preterm infants requires addressing these challenges.
Factors Affecting TcB Accuracy
Several factors influence the accuracy of TcB measurements in premature infants:
- Gestational Age (GA): Prematurity is a major factor. The younger the infant, the less reliable the TcB reading may be. This is likely due to variations in skin thickness, hydration, and bilirubin distribution. Very low birth weight (VLBW) infants are particularly susceptible to inaccuracies.
- Skin Pigmentation: Skin color can affect light absorption and, consequently, TcB readings. Further research is needed to fully understand and compensate for this effect. Ideally, TcB devices should be equipped with algorithms that adjust for variations in skin pigmentation.
- Device Calibration and Operator Skill: Proper calibration of the TcB device and the expertise of the operator are essential for minimizing measurement errors. Training and standardization are key. Healthcare professionals should receive comprehensive training on proper measurement technique, device maintenance, and interpretation of results.
- Ambient Light: Exposure to ambient light can interfere with TcB measurements. Careful control of lighting conditions is crucial. Measurements should be performed in a dimly lit environment to minimize interference from external light sources.
- Hypotension: Fluctuations in blood pressure (hypotension being of particular concern among preemies) may impact TcB readings. This warrants further investigation. Monitor blood pressure and other vital signs when interpreting TcB measurements in premature infants.
- Phototherapy: Exposure to phototherapy can bleach the skin and affect TcB readings. Avoid performing TcB measurements on areas of skin that have been directly exposed to phototherapy. Shielded areas, such as the forehead covered by a mask, are preferred.
Strategies for Improving TcB Accuracy
How to improve transcutaneous bilirubinometry accuracy in premature infants involves a multi-pronged approach:
- Optimal Device Selection: Choose a TcB device validated for use in premature infants, ideally one with algorithms specifically designed to account for age and skin pigmentation. Consult published studies and expert recommendations to guide device selection.
- Strict Adherence to Manufacturer’s Instructions: Follow the manufacturer’s instructions meticulously for device calibration, measurement technique, and data interpretation. This includes controlling ambient light and ensuring proper skin contact. Deviation from the manufacturer’s instructions can compromise accuracy.
- Calibration and Maintenance: Regularly calibrate the TcB device according to the manufacturer’s recommendations. Regular maintenance prevents device malfunction and ensures reliable readings. Implement a routine calibration schedule and document all maintenance activities.
- Operator Training: Ensure healthcare professionals are adequately trained in the correct use of the TcB device and its interpretation of readings. Conduct regular training sessions and competency assessments to ensure proficiency.
- Integration of Machine Learning Models: Emerging machine learning algorithms show promise in correcting TcB errors caused by gestational age and skin pigmentation. Incorporating these models would significantly enhance accuracy.
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026