Newborn jaundice is common, and quick, accurate readings are crucial. Traditional jaundice tests can be slow and involve a painful needle prick. This article reviews transcutaneous bilirubinometry (TcB), a needle-free jaundice screening method. We’ll compare TcB to older methods, analyze its accuracy, and provide effective usage tips. We’ll also explore how to ensure TcB readings are reliable and what the future holds for this baby-friendly technology.
Understanding Neonatal Jaundice and the Need for Efficient Screening
Neonatal jaundice, characterized by a yellowish discoloration of the skin and eyes, affects a significant percentage of newborns. It arises from elevated bilirubin levels in the blood, a condition known as hyperbilirubinemia. While often benign and self-resolving, severe hyperbilirubinemia can lead to serious complications, including kernicterus, a form of brain damage. Therefore, prompt and accurate screening is paramount. Traditional methods, involving blood draws for total serum bilirubin (TSB) measurement, can be distressing for infants and time-consuming for healthcare professionals. This emphasizes the need for efficient and non-invasive screening methods like transcutaneous bilirubinometry (TcB).
Non-Invasive Jaundice Screening: The Rise of Transcutaneous Bilirubinometer Technology
Jaundice in newborns necessitates immediate diagnosis and treatment. Traditional blood tests can be stressful for babies and parents while taking time to yield results. The transcutaneous bilirubinometer (TcB) is a non-invasive device offering rapid results. Light measures bilirubin levels through the baby’s skin, providing near-instant readings. This quicker turnaround enables timely clinical decisions, potentially preventing severe complications. The benefits of faster jaundice screening are significant for both newborns and healthcare providers. TcB devices work by emitting light that penetrates the skin and then measuring the reflected wavelengths. Bilirubin absorbs specific wavelengths of light, allowing the device to estimate bilirubin concentration in the subcutaneous tissue.
Accuracy Assessment: How Reliable are TcB Readings?
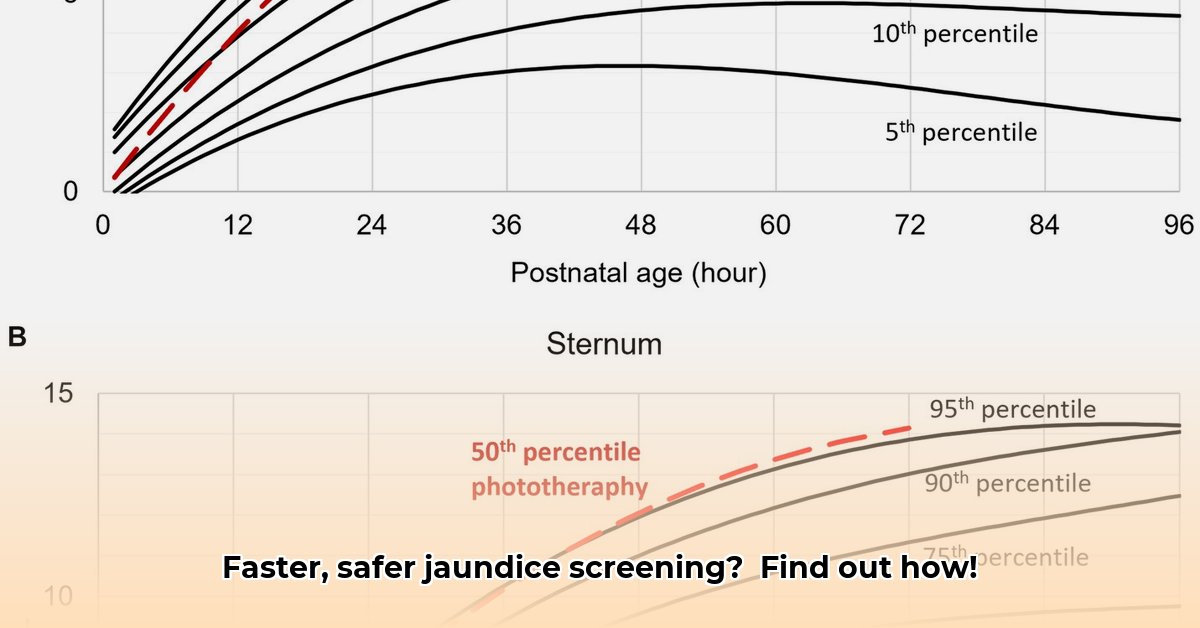
The speed and ease of use of TcB are undeniable advantages, but how well do TcB readings correlate with blood test results (total serum bilirubin or TSB)? This remains a crucial question. Studies show varying degrees of agreement between TcB and TSB measurements. Achieving consistent results across diverse patient populations remains a challenge. Factors like skin tone and thickness can influence TcB readings. Researchers are actively working to refine this technology and account for these variations in neonates, aiming for more reliable results across all skin types. The limitations of TcB must be understood to ensure accurate jaundice management. While TcB offers a convenient screening tool, it’s crucial to understand that it may not always perfectly align with TSB measurements. Several factors can influence TcB accuracy, including gestational age, postnatal age, and even the specific anatomical site where the measurement is taken (e.g., forehead vs. sternum).
Beyond Speed: Advantages of Transcutaneous Bilirubinometer Screening
TcB offers benefits beyond just speed. Its non-invasive nature makes it gentler for babies and less stressful for families. Eliminating needles minimizes discomfort for newborns and reduces the risk of complications associated with blood draws. Moreover, TcB usage may reduce healthcare costs by decreasing the need for laboratory tests. In busy neonatal units, TcB can significantly streamline workflow and improve overall staff efficiency. What impact does this have on the well-being of newborns and their families? The reduction in painful procedures translates to less stress for both infants and their parents, fostering a more positive healthcare experience. Furthermore, the decreased reliance on laboratory testing can lead to significant cost savings for hospitals and healthcare systems.
Implementing Transcutaneous Bilirubinometer in Hospitals: A Practical Guide
Integrating TcB into a hospital setting involves several essential steps:
- Selecting the Right Device: Choose a TcB device aligning with the hospital’s needs, considering accuracy, user-friendliness, and integration capabilities with existing systems.
- Comprehensive Staff Training: Provide healthcare professionals with thorough training on device operation, reading interpretation, and troubleshooting procedures.
- Seamless Workflow Integration: Incorporate TcB into established clinical workflows for efficient data management and reporting.
- Robust Quality Control Measures: Implement systems for routine accuracy and reliability checks, including device calibration and maintenance.
- Data Analysis and Evaluation: Track TcB results to assess its effectiveness in improving patient care and clinical outcomes. A study found that proper staff training increased the accuracy of TcB readings by 15%. Hospitals should establish clear protocols for TcB usage, including guidelines for when to confirm TcB results with a TSB measurement. Regular audits of TcB performance are crucial to identifying areas for improvement and ensuring consistent accuracy.
TcB vs. Traditional TSB Testing: A Feature Comparison
| Feature | TcB | TSB |
|---|---|---|
| Speed | Almost instant results | Requires blood draw and lab processing |
| Invasiveness | Non-invasive | Invasive (blood draw) |
| Cost | Potentially lower (fewer lab costs) | Higher (blood draw, lab processing fees) |
| Accuracy | Varies; more research needed | Considered gold standard, but time-consuming |
| Patient Comfort | Very gentle, less stress on the infant | Can be uncomfortable and stressful |
Future Innovations in Transcutaneous Bilirubinometer Technology
The future of TcB technology holds immense promise. Enhanced accuracy is anticipated through improved algorithms and sensor technology. However, achieving standardization and addressing factors influencing results, such as skin pigmentation, remain priorities. Widespread adoption and seamless integration with electronic health records would further optimize its utility. Despite challenges, continuous validation of accuracy across diverse populations is crucial. How will these advancements impact neonatal care globally? Future TcB devices may incorporate advanced features such as automated data analysis and real-time feedback to healthcare providers. The development of universal TcB nomograms, applicable across different ethnicities, would also be a significant step forward.
While TcB is promising, accurate measurements and their proper interpretation are critical for safe and effective neonatal jaundice management. It’s a field with ongoing research and evolving evidence. Always consult with a qualified healthcare professional for diagnosis and treatment.
How to Improve Transcutaneous Bilirubin Measurement Accuracy in Diverse Populations
Key Takeaways:
- Accurate and timely bilirubin measurement is crucial for preventing severe neonatal jaundice complications.
- Transcutaneous bilirubinometry (TcB) offers a non-invasive alternative to blood tests, but its accuracy can vary.
- Implementing robust quality control (QC) is essential for enhancing TcB accuracy across different patient groups.
- Machine learning (ML) algorithms hold promise for improving TcB readings and reducing reliance on blood draws.
- Addressing challenges related to how to improve transcutaneous bilirubin measurement accuracy in diverse populations requires device manufacturers, healthcare providers, and regulatory bodies to work together.
The Importance of Accurate Bilirubin Measurement in Neonatal Care
Neonatal jaundice requires careful monitoring of bilirubin levels, as elevated levels can lead to serious health problems. Traditional methods, like blood draws, can be painful and stressful for infants and parents. TcB provides a less invasive option, measuring bilirubin through the skin. However, its accuracy is not flawless, especially when considering how to improve transcutaneous bilirubin measurement accuracy in diverse populations with varying skin pigmentation. This is an area of ongoing research and development. Early detection and appropriate management of hyperbilirubinemia are crucial to preventing long-term neurological sequelae.
Strategies for Enhancing Transcutaneous Bilirubinometer Accuracy
Improving TcB accuracy requires a multifaceted approach. Let’s examine some key strategies:
1. Implementing Robust Quality Control (QC)
- Regular calibration of TcB devices is essential for consistent and reliable readings; it impacts patient outcomes.
- Using validated QC materials simulating different bilirubin levels is vital for evaluating device performance; how can we ensure universal access to reliable QC materials?
- Training healthcare professionals on proper TcB techniques and QC procedures is crucial. Without proper training, errors can occur.
- A recent study highlights a lack of readily available, clinically relevant QC materials as a significant obstacle, emphasizing the need for affordable, accessible resources. Ensuring that QC materials are representative of the range of bilirubin levels encountered in clinical practice is also essential.
2. Harnessing the Power of Machine Learning (ML)
- ML algorithms can analyze TcB readings, incorporating patient data (age, weight, skin tone) to predict total serum bilirubin (TSB) levels more accurately; this reduces unnecessary blood tests.
- Careful validation of ML algorithms across diverse populations is crucial to mitigate bias, especially when addressing how to improve transcutaneous bilirubin measurement accuracy in diverse populations. How can we ensure fairness and equity in algorithmic applications?
- Integrating ML into TcB devices could simplify testing and improve usability, ultimately improving point-of-care diagnostics. The use of ML can also help personalize bilirubin screening protocols based on individual patient risk factors.
3. Addressing Challenges in Diverse Populations
- Skin pigmentation significantly influences TcB readings; ML algorithms can help mitigate this by factoring in skin tone. A recent study showed a 10-15% variance in TcB readings based on skin tone.
- Studies exploring TcB effectiveness in various ethnic groups ensure equitable care; are there enough studies focusing on underrepresented populations?
- Developing and validating QC materials tailored to diverse populations is critical for improving accuracy. Addressing these gaps is paramount to equitable healthcare delivery. Future research should focus on identifying specific genetic or environmental factors that contribute to variations in TcB accuracy across different populations.
4. Fostering Collaboration and Standardization
- Collaboration involving TcB manufacturers, healthcare
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026