Got an ECG report that looks a little strange? Don’t panic! Heart readings can be confusing, but understanding them is key to staying healthy. This guide will help you decipher your ECG results, explaining what’s normal and what’s not in plain English. We’ll cover everything from minor variations to more serious heart issues, and show you what steps you can take next. You’ll gain a better understanding of potential risks and how to keep your heart in optimal condition. For more in-depth information, see this helpful guide on abnormal ECG meanings. Let’s get started!
What Does Abnormal ECG Mean? Decoding Heart Rhythms and Electrical Activity
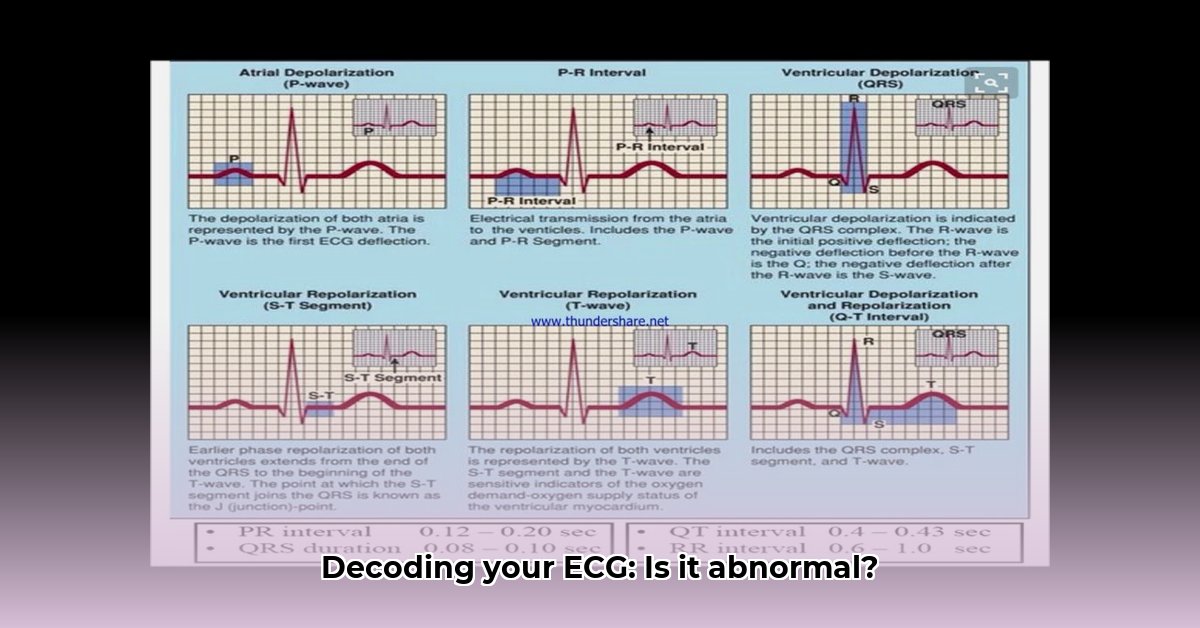
Let’s delve into electrocardiograms, or ECGs (sometimes called EKGs). Think of an ECG as a quick, non-invasive snapshot of your heart’s electrical activity. It’s a simple test that records your heart’s rhythm and how well it’s pumping blood. But what happens when the doctor says your ECG is “abnormal?” Does that automatically mean something’s seriously wrong? Quite often, it doesn’t. Sometimes, minor variations appear that are perfectly normal for you.
Decoding Your ECG: Understanding Your Heart’s Electrical Language
Your doctor is the expert at reading ECGs. They analyze the patterns in the electrical signals to understand how your heart is working. An unusual ECG tracing might reveal problems with your heart rate (how fast or slow your heart beats), its rhythm (whether it beats regularly), or the way electrical signals travel through your heart muscle. These irregularities can point to a range of different things, from benign variations to conditions requiring further investigation.
Reasons Why Your ECG Might Look Different: Common Heart Irregularities and Influencing Factors
There are numerous reasons why your ECG might show something unexpected. Here are a few common ones:
- Heart Rhythm Problems (Arrhythmias): Your heart might beat too fast (tachycardia), too slow (bradycardia), or with an irregular beat. Imagine its rhythm as a drumbeat—sometimes the beat is too fast, too slow, or skips a beat. Common arrhythmias include atrial fibrillation, atrial flutter, and supraventricular tachycardia.
- Heart Attacks (Myocardial Infarctions): A heart attack damages part of your heart muscle, which disrupts the electrical signals. The ECG will often reflect this damage. A heart attack is a serious medical emergency requiring immediate help.
- Electrolyte Imbalances: Electrolytes, such as potassium, calcium, and magnesium, are essential minerals that are vital for your heart’s electrical function. If your levels are off—too high or too low—it can disrupt the signals, which will show up on your ECG.
- Heart Valve Problems: Your heart has valves that control the flow of blood. If these valves aren’t working correctly (stenosis or regurgitation), they can impact your heart’s electrical activity.
- Heart Muscle Diseases (Cardiomyopathies): These conditions affect your heart muscle’s ability to pump blood efficiently. This, in turn, can affect the electrical signals and potentially lead to arrhythmias. Examples include hypertrophic cardiomyopathy and dilated cardiomyopathy.
- Medications: Some medications, including certain antidepressants, antihistamines, and decongestants, can affect your heart rhythm and show up on an ECG. Always inform your doctor of all medications you are taking.
- Birth Defects (Congenital Heart Defects): Some people are born with heart conditions that can cause an abnormal ECG. These defects can affect the heart’s structure and electrical pathways.
- Pulmonary Embolism: Although not a direct heart condition, a pulmonary embolism (blood clot in the lungs) can strain the heart and lead to ECG changes.
- Chronic Lung Disease: Conditions like COPD can sometimes cause changes on an ECG due to increased pressure in the chest cavity.
What Happens After an Abnormal ECG? Further Heart Investigations and Diagnostic Procedures
Finding an abnormality on your ECG doesn’t automatically mean you’re seriously ill. It simply means your doctor needs more information to determine the cause and significance. They’ll consider your symptoms, medical history, and other risk factors before reaching a diagnosis. They might recommend more tests to get a clearer picture. These additional tests could include:
- Echocardiogram: This uses sound waves to create moving pictures of your heart, showing how well the chambers are pumping and how the valves are functioning. Think of it like an ultrasound for your heart.
- Stress Test: This involves exercising (or using medication to simulate exercise) while your heart’s activity is monitored. It helps determine if your heart is functioning well under stress and if there are any signs of ischemia (reduced blood flow).
- Holter Monitor: This is like a portable ECG you wear for 24-48 hours (or longer in some cases). It continuously records your heart’s rhythm, capturing a much longer view compared to the snapshot of a regular ECG. This is useful in detecting intermittent arrhythmias.
- Event Monitor: Similar to a Holter monitor, but worn for a longer period (weeks to months). It records heart activity only when triggered by the patient or when it detects an abnormal rhythm.
- Cardiac Catheterization: A more invasive procedure where a catheter is inserted into a blood vessel and guided to the heart. It allows doctors to measure pressures in the heart chambers and visualize the coronary arteries.
Understanding Your Results: Personalized Heart Analysis and Interpretation
Getting an abnormal ECG result can be concerning. It’s crucial to remember that the ECG is only one piece of the puzzle. Your doctor will use it along with everything else they know about you, such as your symptoms, medical history, and other test results, to figure out what’s going on.
Here are some possible scenarios:
- It’s Likely Nothing to Worry About: In many cases, an abnormal ECG finding is simply a minor variation that’s completely harmless. Many healthy people have minor variations on their ECG. These variations may be due to body habitus, normal physiological changes with age, or other benign factors.
- There’s an Underlying Condition That Needs Monitoring: Sometimes, an abnormal ECG suggests an underlying heart condition that doesn’t require immediate treatment but needs to be monitored over time. This might involve regular check-ups and repeat ECGs.
- There’s an Underlying Condition Requiring Treatment: In some cases, an abnormal ECG points to a condition that needs to be treated with lifestyle changes, medication, or potentially more invasive procedures like angioplasty or surgery.
Your doctor is the only one who can accurately interpret your specific ECG results and explain what they mean for your health. Talk to them openly; ask questions until you understand the findings, the potential causes, and the recommended course of action.
Living Well with Your Heart: Heart Health Lifestyle and Preventative Measures
No matter what your ECG shows, maintaining a heart-healthy lifestyle is essential for your overall well-being. Here’s how:
- Get Regular Exercise: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous-intensity aerobic activity per week, or a combination of both. Include muscle-strengthening activities at least two days a week.
- Eat a Balanced Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins. Limit saturated and trans fats, cholesterol, sodium, and added sugars. The Mediterranean diet is a great example of a heart-healthy eating pattern.
- Maintain a Healthy Weight: Being overweight or obese increases your risk of heart problems, including high blood pressure, high cholesterol, and diabetes.
- Manage Stress: Chronic stress can negatively impact your heart health. Find healthy ways to cope with stress, such as yoga, meditation, spending time in nature, or engaging in hobbies you enjoy.
- Don’t Smoke: If you smoke, quit! Smoking dramatically increases your risk of heart disease, stroke, and other health problems.
- Limit Alcohol Consumption: If you drink alcohol, do so in moderation. This means up to one drink per day for women and up to two drinks per day for men.
- Get Enough Sleep: Aim for 7-8 hours of quality sleep per night.
- Regular Check-ups: See your doctor regularly for check-ups, including blood pressure and cholesterol screenings.
- Know Your Family History: Understanding your family history of heart disease can help you assess your risk and take preventative measures.
Remember, an abnormal ECG isn’t a diagnosis on its own. It’s a signal that more investigation may be needed. Your doctor is your best source of information and support. Don’t hesitate to discuss your concerns and ask questions—it’s your heart health, after all.
How to Interpret Asymptomatic Abnormal EKG Results in Athletes: Athletic Heart ECG
Understanding an abnormal EKG (electrocardiogram) can be particularly challenging for athletes. A seemingly minor irregularity might simply reflect the physiological adaptations to intense training, or it could signal a potentially serious underlying heart condition. This guide helps you navigate the complexities of how to interpret asymptomatic abnormal EKG results in athletes, focusing on distinguishing normal variations from potential problems.
What’s Normal for an Athletic Heart? Athletic Heart Adaptations and Physiological Changes
Your heart adapts to the demands of strenuous exercise. Regular athletic training often leads to structural and electrical changes that can mimic disease patterns. These adaptations aren’t necessarily cause for alarm. Common “normal abnormalities” in athletes include:
- Slow heart rate (bradycardia):
- Portable Hydroelectric Generators Harness Nature for Off-Grid Power - February 21, 2026
- Generate Free Electricity for Home From Renewable Sources - February 18, 2026
- Micro-Hydro Offers Cheapest Home Electricity if You Have a Stream - February 17, 2026