Is your little one looking a bit yellow? Newborn jaundice is more common than you might think, and understanding it is key to keeping your baby healthy. This guide will walk you through everything you need to know about bilirubin – that yellow pigment that can sometimes cause jaundice in babies. We’ll explain the different types of jaundice, how to spot it, what causes it, and what to do if you have concerns. We’ll cover when to call the doctor, treatment options, and even how to help your baby’s body get rid of the excess bilirubin. Whether you’re a parent wanting to be prepared or a healthcare professional looking for a detailed overview, this guide provides clear, comprehensive information to ensure your baby gets the best care. For more detailed information on interpreting jaundice results, check out this helpful resource: Understanding Jaundice Results.
Understanding Neonatal Jaundice: Key Information and Insights
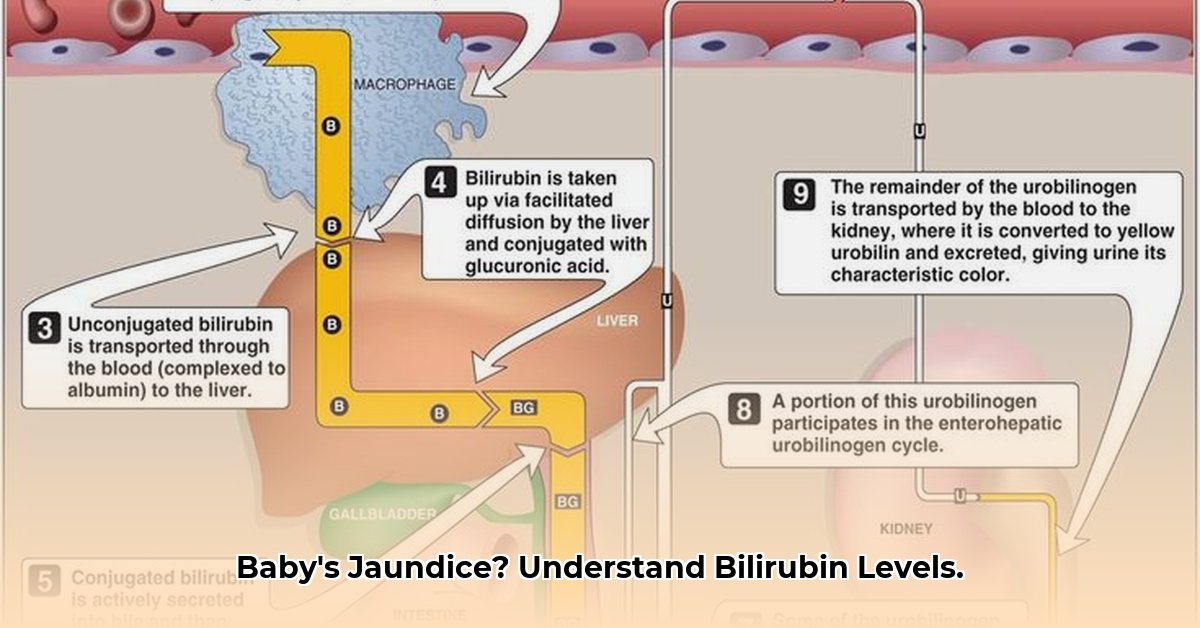
Jaundice, characterized by a yellowish color on a baby’s skin and the whites of their eyes, occurs when a substance called bilirubin accumulates in the blood. Bilirubin is a natural byproduct produced when the body breaks down old red blood cells. A newborn’s liver, still in its developmental stages, may not be fully efficient at processing and removing bilirubin, leading to a temporary yellowish tint. While often harmless, monitoring your baby’s bilirubin levels is essential. Understanding these levels is crucial for infant health and well-being.
Understanding Jaundice: It’s More Common Than You Think
Newborn jaundice is a prevalent condition, affecting a significant percentage of newborns. In many cases, it is benign and resolves spontaneously within a couple of weeks. The underlying reason is that a baby’s liver is immature and still developing the capacity to efficiently process bilirubin. However, in some instances, elevated bilirubin levels can indicate an underlying issue that warrants medical attention. Early identification of jaundice and appropriate intervention can significantly improve health outcomes.
Different Types of Jaundice: Knowing the Nuances
Jaundice presents in several forms, each with distinct underlying factors:
- Physiological Jaundice: This is the most frequently observed type of newborn jaundice. It typically poses no significant health risks. The baby’s liver requires time to mature fully and effectively eliminate bilirubin. It represents a normal adaptive process during the newborn period.
- Breastfeeding Jaundice: This type is associated with the frequency and effectiveness of breastfeeding. Inadequate or infrequent feedings can lead to dehydration and reduced bilirubin excretion. Encouraging more frequent feedings can usually resolve this issue. Proper latch and regular nursing sessions are critical factors.
- Breast Milk Jaundice: This condition differs from breastfeeding jaundice. Specific components present in breast milk can affect how bilirubin is processed by the infant’s liver, leading to a prolonged yellow tinge. This condition is usually benign, but monitoring remains important.
- Pathological Jaundice: This form necessitates immediate medical intervention. It suggests the presence of an underlying medical condition, such as an infection, blood incompatibility between mother and baby, or a liver disorder. Pathological jaundice often manifests within the first 24 hours of life, requiring prompt diagnosis and treatment.
What Causes Jaundice? Delving Deeper
Several factors can contribute to the development of jaundice in newborns:
- Immature Liver Function: As mentioned earlier, the primary cause is the newborn’s liver not being fully developed.
- Increased Red Blood Cell Breakdown: Newborns have a higher concentration of red blood cells, which break down more quickly than in adults.
- Reabsorption of Bilirubin: The infant’s intestines may reabsorb bilirubin before it can be excreted.
- Certain Medical Conditions: As mentioned above, infections, blood incompatibilities, and liver abnormalities can cause jaundice.
Who’s at Higher Risk? Identifying Potential Factors
Specific factors elevate the likelihood of a baby developing higher bilirubin levels. Awareness of these risk factors enables healthcare providers to deliver tailored monitoring:
- Premature Babies: Premature infants possess less developed livers, rendering them more susceptible to bilirubin accumulation.
- Ethnicity: Infants of East Asian or Mediterranean descent may exhibit a slightly increased risk, although further research is ongoing to understand these disparities.
- Significant Bruising During Birth: Trauma sustained during delivery can sometimes result in elevated bilirubin levels.
- Blood Type Incompatibilities: When the mother’s and baby’s blood types are incompatible (Rh incompatibility or ABO incompatibility), the likelihood of jaundice increases.
- Infections: Maternal infections contracted during pregnancy may impact neonatal bilirubin levels.
- Genetic Conditions: Certain inherited conditions, such as Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency and Gilbert’s Syndrome, are associated with an elevated risk of jaundice.
Spotting Jaundice: What to Watch For
The most obvious sign of jaundice is yellowing of the skin and the whites of the eyes. This yellowing usually starts on the face and then spreads down to the chest, abdomen, arms, and legs.
Other signs and symptoms can include:
- Poor feeding
- Lethargy
- Dark urine
- Pale stools
Jaundice can be harder to see in babies with darker skin tones. In these cases, check the gums and whites of the eyes.
Measuring Bilirubin: How Doctors Get a Read
Physicians employ several methods to quantify bilirubin levels in newborns:
- Non-invasive Transcutaneous Bilirubin (TcB): This swift and painless test involves utilizing a specialized device to measure bilirubin levels through the skin.
- Total Serum Bilirubin (TSB): This test entails obtaining a small blood sample through a heel prick to ascertain precise bilirubin concentrations.
The obtained results are juxtaposed with age-specific charts tailored to the infant’s age. These charts enable healthcare providers to determine whether bilirubin levels fall within the normal range or warrant intervention. These charts account for gestational age and other influencing factors to ensure accurate assessments.
Treatment: When Intervention is Needed
When an infant’s bilirubin levels exceed acceptable thresholds, healthcare providers may recommend the following treatment options:
- Phototherapy: This therapeutic modality entails exposing the infant to specific wavelengths of blue light, which aids in the breakdown of bilirubin molecules. Infants may require intermittent phototherapy sessions for a designated duration to enhance bilirubin excretion.
- Exchange Transfusion: This complex procedure is reserved for extreme instances of elevated bilirubin levels. It involves gradually replacing the infant’s blood with donor blood, and is quite rare.
- Intravenous Immunoglobulin (IVIG): In cases of Rh incompatibility, IVIG may be used to reduce the breakdown of red blood cells.
Frequent feeding is also key. It helps your baby eliminate bilirubin through their stools. Breastfeeding mothers should aim for very frequent feeding (8-12 times a day), while formula-fed babies should be fed every 2-3 hours. This frequent feeding promotes bowel movements which help remove bilirubin.
What You Can Do: A Guide for Parents
- Be Observant: Closely monitor your baby’s skin and eyes for any signs of yellowish discoloration.
- Feed Often: Encourage frequent breastfeeding or administer formula regularly to sustain hydration and optimize liver function.
- Keep Appointments: Attend all scheduled check-up appointments to facilitate bilirubin level monitoring.
- Communicate: Do not hesitate to address any concerns or queries with your healthcare provider. Seeking clarification is always prudent.
- Proper Hydration: Make sure your baby is getting enough fluids, either through breast milk or formula.
- Sunlight Exposure (with caution): Brief exposure to sunlight can help break down bilirubin, but always avoid direct sunlight and overheating. Consult your doctor before using sunlight as a treatment.
For Healthcare Professionals: Key Considerations
- Risk Assessment: Identify infants at increased risk based on predisposing factors.
- Choosing the Right Test: Determine the most suitable diagnostic method (TcB or TSB) based on the clinical scenario.
- Interpreting Results Carefully: Utilize age-specific charts to ensure precise interpretation of bilirubin levels.
- Acting Promptly: Timely initiation of treatment (phototherapy or exchange transfusion), when indicated, is crucial.
- Educating Parents: Supply parents with accessible and comprehensive information regarding jaundice, its management, and the significance of frequent feeding.
Remember, early detection and proper management are key to preventing potential long-term complications. Trust your instincts and don’t hesitate to reach out to your pediatrician with any questions or concerns. Your peace of mind is crucial, too! Did you know that early detection of jaundice and appropriate management are instrumental in preventing potential long-term complications for your baby?
Understanding the Differences: Breastfeeding Jaundice vs. Breast Milk Jaundice
Jaundice, that yellowish tinge to your baby’s skin and eyes, is surprisingly common. But understanding why your little one is yellow is crucial. It’s not all the same. There are different types of jaundice, each with its own cause and treatment. Let’s explore two related but distinct types: breastfeeding jaundice (BFJ) and breast milk jaundice (BMJ). How to differentiate breastfeeding jaundice from breast milk jaundice in newborns is a question many parents have, and it’s vital to understand the differences for your baby’s well-being. Did you know that distinguishing between breastfeeding jaundice and breast milk jaundice is crucial for ensuring your baby receives the most appropriate care?
Understanding the Types of Jaundice
Physiological jaundice is the most common
- How To Generate Power At Home For Energy Independence - February 4, 2026
- How Can I Produce Electricity At Home Using Renewable Sources? - February 3, 2026
- How To Generate Electricity at Home Using Renewable Energy - February 2, 2026