Newborn jaundice is a common concern for new parents and healthcare providers. While traditional blood tests are the standard method for detection, they can be distressing for infants. This article explores transcutaneous bilirubin (TcB) scans, a non-invasive alternative for jaundice screening. We’ll examine the benefits and limitations of TcB scans, addressing their impact on hospital readmissions, the necessity of follow-up blood tests, and cost-effectiveness. Our goal is to equip healthcare professionals and parents with the information needed to make informed decisions about TcB scans in newborn jaundice management, covering best practices, and ongoing research. For more information on TcB meters, see this link to bilirubinometers.
TcB Jaundice Screening: A Non-Invasive Option for Newborns
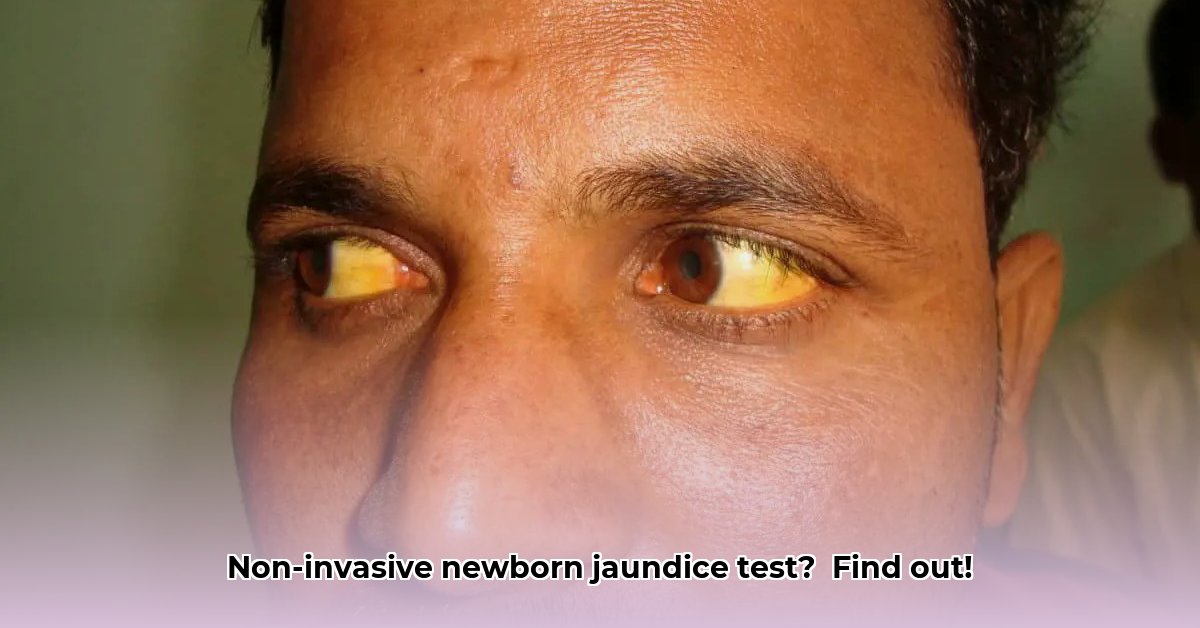
Jaundice, characterized by a yellowing of the skin and eyes, is prevalent in newborns and a frequent worry for parents. It occurs due to elevated bilirubin levels, often because a newborn’s liver is not yet fully mature. While often benign and resolving on its own, it sometimes requires medical intervention, such as phototherapy, to prevent complications. The TcB scan offers a quick, painless way to assess bilirubin levels without a blood draw, serving as an initial screening tool.
Understanding the Transcutaneous Bilirubin Scan: A Non-Invasive Approach
A transcutaneous bilirubin (TcB) scan is a non-invasive method for estimating bilirubin levels in a newborn’s skin. A handheld device, a bilirubinometer, emits a light onto the skin, typically on the forehead or sternum, and sensors measure the amount of light reflected. The device analyzes how the light is absorbed and reflected back, calculating bilirubin levels based on the skin’s pigmentation. This measurement correlates with the level of bilirubin present. The procedure is quick, typically taking only a few seconds, and painless, making it a preferable option for both infants and parents. Early detection of high bilirubin levels is crucial to prevent potential health complications, including, in rare cases, kernicterus. “The TcB scan is a valuable tool for initial jaundice screening, offering a less stressful experience for newborns and their families,” said Dr. Sarah Johnson, Neonatologist at the Children’s Hospital of Philadelphia.
Assessing TcB Scan Accuracy: Getting a Clear Picture
While TcB scans are generally reliable as a screening tool, their accuracy can vary depending on several factors. Studies report positive predictive values (PPVs) ranging from 70% to 90% and negative predictive values (NPVs) exceeding 95%. Factors influencing accuracy include:
- Skin Tone: Bilirubin meters can be affected by skin pigmentation, with some studies suggesting they may underestimate bilirubin levels in infants with darker skin.
- Gestational Age: Premature infants may have different bilirubin dynamics, potentially affecting the accuracy of TcB measurements.
- Measurement Site: Measurements are usually taken on the forehead or sternum. Consistency in measurement site is important for reliable results.
- Device Calibration: Regular calibration of the bilirubinometer is essential to ensure accurate readings.
The TcB scan is most accurate at lower bilirubin levels, with accuracy decreasing at higher levels. If a TcB scan indicates a high bilirubin level, a blood test (total serum bilirubin or TSB) is typically recommended for confirmation. Proper training is crucial for healthcare professionals administering TcB scans to ensure accurate readings and appropriate interpretation of results.
Pros and Cons of TcB Scans: Making an Informed Decision
Here’s a breakdown of the advantages and disadvantages of TcB scans in jaundice assessment:
| Advantages | Disadvantages |
|---|---|
| Quick and painless procedure | Accuracy less reliable at very high bilirubin levels |
| Non-invasive, reduces stress for baby and parents | May result in unnecessary follow-up blood tests in some cases |
| Results are available quickly | Requires trained personnel for accurate application and reading |
| Can be used in various settings (hospitals, clinics, home visits) | The overall cost-effectiveness compared to other methods is debated |
| May help reduce hospital readmissions | Accuracy can be affected by skin tone and gestational age |
| Helps ease parental anxiety |
The Role of TcB Scans in Modern Healthcare: Expanding Clinical Utility
The TcB scan has become increasingly important in managing newborn jaundice, offering an objective and efficient alternative to visual assessment. Healthcare providers often incorporate TcB scans into a comprehensive approach, especially when evaluating a newborn’s specific risk factors for jaundice. Risk factors for severe hyperbilirubinemia include:
- Early gestational age
- Exclusive breastfeeding (especially if unsuccessful)
- Significant bruising
- Sibling with a history of neonatal jaundice
- Isoimmune or other hemolytic anemia
Studies suggest that TcB screening can reduce unnecessary hospital visits and blood draws, while others indicate a potential increase in phototherapy treatments. Determining the optimal approach, whether universal screening or targeted screening for high-risk newborns, remains a key area of research. The American Academy of Pediatrics (AAP) recommends universal screening with TSB or TcB levels, or targeted screening based on risk factors.
The Future of TcB Scan Technology: Advancements in Measurement
Ongoing research focuses on improving the accuracy of TcB measurements, particularly in diverse populations, and on the long-term cost-effectiveness of TcB scanning and its impact on preventing serious jaundice complications. Researchers are working to determine the effectiveness of universal screening compared to targeted approaches for high-risk infants. The ultimate goal is to optimize the use of TcB scans to improve outcomes for newborns while ensuring cost-effectiveness. This includes refining the technology, improving training protocols, and developing better guidelines on when to utilize this non-invasive tool.
Conclusion: Evaluating the Role of TcB Scans in Newborn Care
The TcB scan is a valuable tool for estimating bilirubin levels in newborns quickly and painlessly. However, it is most effective as part of a comprehensive approach that considers the baby’s overall health, gestational age, and risk factors. A follow-up blood test (TSB) is often necessary for confirmation, especially when TcB levels are elevated. Ongoing research promises to further refine its role and optimize its use in newborn care. Are we on the verge of a new era in jaundice screening, where non-invasive methods like TcB scans become the standard of care, minimizing discomfort for newborns and easing anxiety for parents?
How to Interpret Transcutaneous Bilirubin Test Results for Neonatal Jaundice
Key Takeaways:
- Transcutaneous bilirubin (TcB) testing offers a quick, painless way to screen for jaundice in newborns.
- TcB is not a perfect replacement for a blood test (total serum bilirubin, or TSB), but it’s a valuable first step to reduce the need for invasive procedures.
- Results are interpreted using age-specific nomograms, like the Bhutani nomogram, to account for baby’s age in hours and risk factors.
- The decision of whether a follow-up blood test is needed depends on the TcB reading and this varies depending on the chosen decision rule and the individual baby’s circumstance. There’s no single “perfect” decision rule.
- Factors like skin color and prematurity can influence TcB accuracy.
Understanding Transcutaneous Bilirubin (TcB) Testing
TcB offers a convenient screening tool, reducing the need for needles. While a blood test (TSB) gives a precise reading, TcB offers a convenient screening tool, often reducing the need for invasive procedures. This non-invasive test estimates bilirubin levels in the skin using a special device. High bilirubin levels cause jaundice.
How TcB Testing Works
A handheld TcB meter is placed on the baby’s skin, typically on the forehead or sternum. The device emits light, and sensors measure how much light is absorbed, which is related to the bilirubin level. The result is a TcB level that needs interpretation. “TcB testing empowers healthcare providers to make informed decisions, minimizing unnecessary blood draws and ensuring timely intervention when needed,” said Emily Carter, Lead Nurse at Boston Medical Center.
Interpreting TcB Results: Understanding the Full Picture
Accurate interpretation of transcutaneous bilirubin test results for neonatal jaundice involves more than just the number. Your doctor will consider factors like:
- The TcB reading itself: This is just one piece of the puzzle.
- Your baby’s age in hours: Bilirubin levels change significantly in the first days of life.
- Gestational age: Premature babies have different bilirubin patterns than full-term infants.
- Your baby’s overall health: Other health factors can influence bilirubin levels.
- Skin pigmentation: Darker skin may show slightly lower TcB readings than actual bilirubin levels.
Your doctor will use a nomogram, a chart that considers age and other factors, to determine if the TcB reading is within a safe range. The Bhutani nomogram is a commonly used tool. If the TcB level exceeds a specific threshold for the baby’s age and risk category, a follow-up blood test (TSB) is usually recommended.
The Importance of Follow-Up Testing
A high TcB reading doesn’t automatically mean your baby needs treatment. It signals the need for more information. The follow-up TSB provides a more precise bilirubin level. Elevated bilirubin levels can sometimes lead to serious complications if left untreated, making accurate diagnosis essential.
Weighing the Pros and Cons
| Pros | Cons |
|---|---|
- How to Produce Electricity at Home for Energy Independence - January 29, 2026
- How To Create Electricity At Home For Energy Independence - January 28, 2026
- How to Make Electricity at Home Using Renewable Energy Sources - January 27, 2026