Newborn jaundice, characterized by elevated bilirubin levels (a yellowish pigment), is a common concern for parents and pediatricians. Phototherapy, a light treatment to reduce bilirubin levels, is generally safe and effective. This article clarifies how phototherapy supports newborns with hyperbilirubinemia, its implementation, and the importance of maintaining appropriate bilirubin levels. This guide reflects updated guidelines, helping optimize your baby’s present and future health. For more information on bilirubin levels, see this helpful resource: infant bilirubin levels.
Phototherapy Threshold Bilirubin: A Parent’s Guide to Understanding Jaundice
Let’s explore newborn jaundice, concentrating on the bilirubin levels that prompt healthcare professionals to recommend phototherapy. Understanding the fundamentals of this treatment can significantly reduce anxiety for new parents. The goal is to proactively address potential complications while ensuring your baby’s comfort and well-being.
Defining the “Threshold”: Individualized Care for Every Baby
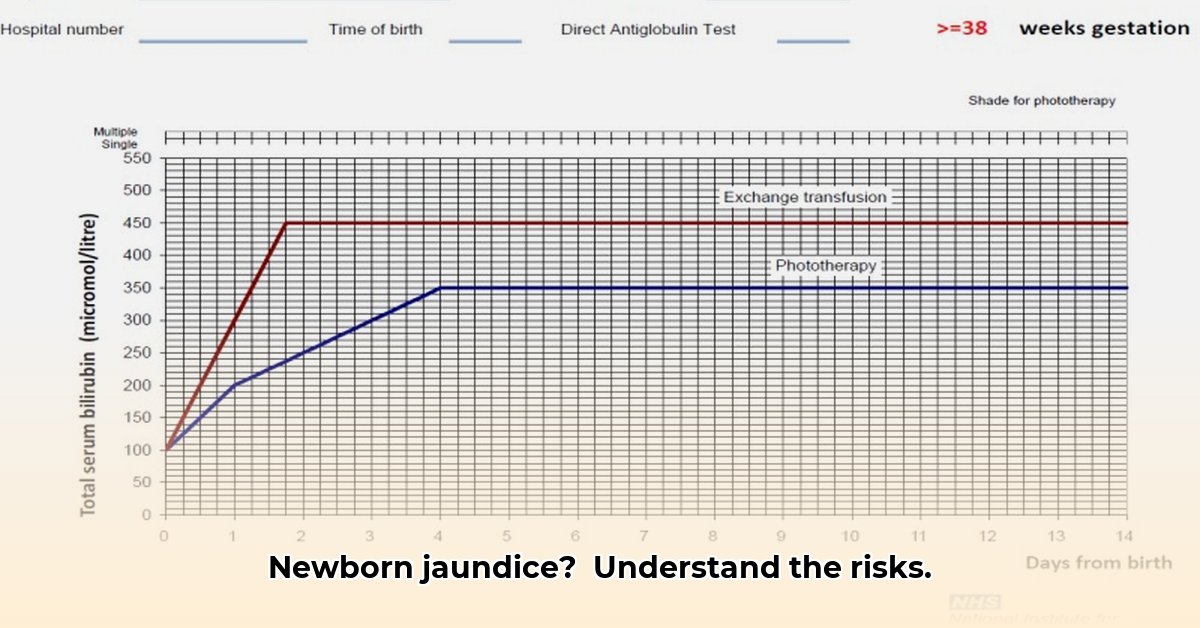
The bilirubin level that triggers phototherapy isn’t a one-size-fits-all number; it varies based on each baby’s unique circumstances. A premature infant will have different needs and a different phototherapy threshold compared to a full-term infant. Doctors consider various factors to create individualized treatment plans, aiming for the most appropriate intervention for each baby.
Elevated bilirubin levels can, in rare instances, lead to kernicterus, a type of brain damage. Phototherapy uses specialized lights to help the body break down bilirubin, preventing this complication. Through continuous monitoring, phototherapy is administered only when the benefits outweigh the risks, minimizing unnecessary interventions.
Factors Influencing Phototherapy Decisions
When considering phototherapy, healthcare providers take into account several elements:
- Age (in hours): Bilirubin levels typically rise in the first few days of life. Phototherapy thresholds increase as the baby gets older, reflecting this natural progression.
- Gestational Age: Preterm infants often require phototherapy sooner than full-term babies because their livers may be less developed, impacting their ability to process bilirubin. Close monitoring is critical.
- Feeding Method: Breastfed babies may exhibit slightly higher bilirubin levels than formula-fed babies. This isn’t always a cause for concern and doesn’t automatically necessitate phototherapy. Continued exclusive breastfeeding is often encouraged.
- Underlying Health Conditions: Blood type incompatibilities (Rh or ABO), G6PD deficiency, or other health issues can increase the risk of hyperbilirubinemia. Doctors may consider phototherapy at lower bilirubin levels in these cases.
- Risk Factors: presence of bruising, cephalohematoma, sibling with history of jaundice requiring phototherapy
Understanding Bilirubin Tests: TSB vs. TcB Explained
Doctors measure bilirubin using TSB (Total Serum Bilirubin) or TcB (Transcutaneous Bilirubin). TSB, a blood test, provides a precise measurement of total bilirubin. TcB, a skin scan, estimates bilirubin levels non-invasively. While TcB is convenient, TSB remains the gold standard due to its accuracy. The decision to initiate phototherapy relies heavily on these measurements, which require careful interpretation by healthcare professionals.
Guidelines: A Delicate Balance
Phototherapy initiation guidelines generally agree on these key points:
- Universal Screening: Routine bilirubin level checks before hospital discharge are considered essential.
- Individualized Approach: No one-size-fits-all approach exists; individual health factors must guide decisions.
- Post-Discharge Monitoring: Continued observation and testing may be necessary after discharge to ensure bilirubin levels remain within a safe range.
Phototherapy: What Parents Can Expect
Phototherapy involves placing the baby under special lights, which aid the body in breaking down bilirubin more efficiently. During treatment, babies wear eye protection. Healthcare providers will monitor the baby’s temperature and hydration. Hospitals often provide resources to support parents. “Many hospitals offer comprehensive support and resources to help parents feel more comfortable during this treatment,” explains [Dr. Emily Carter, Lead Pediatrician] at [UCLA Mattel Children’s Hospital].
Staying Informed and Engaged in Your Baby’s Care
Don’t hesitate to ask your doctor questions about bilirubin levels or phototherapy. Open communication ensures optimal care for your baby. Actively participate in every step of the decision-making process.
The Future of Jaundice Management: Ongoing Research and Advancements
Research continues to refine our understanding of jaundice management. New information may lead to evolving guidelines. Stay informed through reputable sources like the American Academy of Pediatrics and the National Institutes of Health.
Important Note: This article is for informational purposes only and does not substitute professional medical advice. Always consult with your physician or other qualified healthcare provider.
Interpreting Research on Long-Term Neurological Outcomes of Neonatal Hyperbilirubinemia
Neonatal hyperbilirubinemia (NHB), or jaundice, is common in newborns, and while usually harmless, it can raise concerns about long-term effects. How can we interpret conflicting research on this topic?
Understanding the Challenges in Researching Long-Term Effects
The relationship between NHB and later neurodevelopmental issues isn’t always clear. Factors like premature birth, genetic predispositions, and other health concerns can complicate the picture, making it challenging to isolate bilirubin’s specific effects. Studies also differ in how they measure bilirubin levels and neurodevelopment, creating comparison challenges.
Making Sense of the Data: A Critical Approach
Interpreting conflicting research on the long-term neurological impacts of neonatal hyperbilirubinemia requires a critical, discerning approach. Consider these factors:
- Study Population: Were the babies premature, full-term, or did they have other health problems?
- Methods: How did researchers measure bilirubin levels and assess neurodevelopment? What tools and techniques were used?
- Sample Size: Was the study large enough to draw reliable conclusions? Larger studies provide stronger evidence.
- Statistical Analysis: Did researchers use appropriate statistical methods to account for confounding factors, such as prematurity or other medical conditions?
- Publication Bias: Studies that find a link between NHB and neurodevelopmental problems may be more likely to be published than those that don’t. This can skew the overall picture.
- Follow-up Duration: How long were the children followed to assess neurodevelopment outcomes? Longer follow-up periods provide a more comprehensive understanding of potential long-term effects.
What Current Research Shows
While many questions remain, experts agree that extremely high bilirubin levels (leading to kernicterus) cause brain damage. Even milder forms of NHB may increase the risk of some developmental delays in some infants, particularly premature ones. Generally, phototherapy effectively prevents serious problems.
Moving Forward with Research and Clinical Practice
More research is needed, particularly large, well-designed studies that control for other factors. Standardized methods for measuring bilirubin and assessing neurodevelopment would also help facilitate study comparability.
Key Takeaways for Parents:
- Mild to moderate NHB does not automatically equate to long-term neurodevelopmental problems.
- Premature babies may be at higher risk and require closer monitoring.
- Monitoring is crucial for all newborns, especially those with risk factors.
- Phototherapy is generally effective and safe for treating elevated bilirubin levels.
- Interpreting conflicting research requires critical evaluation of study design and methodology; consult your pediatrician for personalized guidance.
How Breastfeeding Practices Influence Phototherapy Thresholds in Neonates
Breastfeeding practices can significantly influence phototherapy thresholds. Key points to consider include:
- Updated guidelines emphasize proactive prevention and early detection of newborn jaundice.
- Universal bilirubin screening before hospital discharge is strongly recommended.
- Treatment approaches are carefully tailored based on individual risk factors.
- Further research is needed to understand the long-term effects of phototherapy on breastfeeding duration and success.
- Resource disparities within healthcare systems can affect guideline implementation and access to optimal care.
- Early identification of Glucose-6-Phosphate Dehydrogenase (G6PD) deficiency remains a significant challenge.
Understanding Neonatal Jaundice: A Brief Overview
Newborn jaundice, medically known as hyperbilirubinemia, occurs when bilirubin builds up in the blood. Mild jaundice usually resolves spontaneously; however, more severe cases require prompt medical intervention.
Phototherapy: A Cornerstone of Jaundice Treatment
Phototherapy utilizes special lights to effectively break down bilirubin. Understanding its complex interplay with breastfeeding practices is crucial for optimizing newborn care.
Breastfeeding’s Pivotal Role
Breastfeeding provides vital nutrients and immunological benefits for a baby’s optimal growth and development. How does it influence the bilirubin levels at which phototherapy becomes necessary?
The American Academy of Pediatrics (AAP) strongly advocates for distinguishing between jaundice caused by inadequate milk intake versus factors present within breast milk itself. These nuances directly affect decisions about phototherapy thresholds. Recent guideline updates have slightly raised thresholds based on emerging scientific evidence.
Research Insights: Exploring the Impact of Breastfeeding Practices on Phototherapy Thresholds
Recent research studies have revealed varied outcomes. Some studies suggest that phototherapy might inadvertently lower rates of exclusive breastfeeding, although this association tends to disappear when researchers control for other contributing factors. The precise long-term impact remains somewhat unclear and necessitates further, ongoing investigation.
Addressing Healthcare Disparities
Implementing these comprehensive guidelines presents challenges due to existing disparities in healthcare resource availability, which in turn affects jaundice management strategies, G6PD deficiency detection rates, and the overall quality of
- How To Generate Power At Home For Energy Independence - February 4, 2026
- How Can I Produce Electricity At Home Using Renewable Sources? - February 3, 2026
- How To Generate Electricity at Home Using Renewable Energy - February 2, 2026